What is antimicrobial resistance (AMR)?
AMR occurs when bacteria develop ways to resist antimicrobial medicines (which include antibiotics). They can do this by (i) developing new, or (ii) changing existing features that would normally make them sensitive to antimicrobials. These resistant bacteria then grow causing very bad and uncontrolled infections. There are limited medicines to treat these bacteria, and sadly the consequences can be deadly.
The World Health Organisation (WHO) has named AMR as one of their top global health priorities, which they predict will cause over 10 million deaths every year within the next 30 years if nothing is done.
Who can be affected by AMR?
AMR can affect anyone. However, certain groups of people, including those with Cystic Fibrosis (CF), Chronic Obstructive Pulmonary Disease (COPD) or those who are immunocompromised (chemotherapy and organ transplant recipients) experience many recurrent bacterial infections. Treatment of these infections with multiple courses of antibiotics over a long time period makes it more likely for resistance to occur in these individuals.
What are Phages?
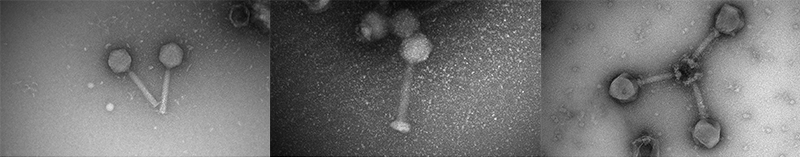
Bacteriophages (phages) are specialised viruses that only kill certain bacteria. They can be found everywhere in the environment, including in waterways and soil.
As humans become more affected by antibiotic resistant bacterial infections, phages can act as “superheroes” in a world where they might have been considered to be “bad guys” just for being viruses. There are millions of different types of phages in the environment; the more we collect and understand how they work, the more bacterial infections we will be able to fight.
Phages are collected and stored in a “phage library”. Researchers from Wal-yan Respiratory Research Centre have built a large phage library, with over 2000 phages specific to several types of bacteria including Pseudomonas aeruginosa (P. aeruginosa), Staphylococcus aureus (S. aureus), Burkholderia cenocepacia (B. cenocepacia), and Acinetobacter baumannii (A. baumannii).
Our library is continually growing and we plan to include phages specific to other bacteria including Enterococcus faecium (E. faecium), Stenotrophomonas maltophilia (S. maltophilia), Non-Tuberculosis mycobacterium (M. abscessus), Escherichia coli (E. coli), Klebsiella pneumoniae (K. pneumoniae), Enterobacter cloacae (E. cloacae) and Achromobacter xylosoxidans (A. xylosoxidans).
How do Phages work?
Phages bind to the surface of bacteria and inject their genetic material (DNA or RNA) inside. They then use the cellular machinery of the bacteria to make more clones of themselves, resembling a mini army inside the bacteria.
When ready, they burst out of the bacteria causing their death. The newly formed army of phages then infect surrounding bacteria, repeating the process until all bacteria are killed.
What is Phage Therapy?
Bacteriophage (phage) Therapy is the treatment of bacterial infections using specific phages. First, the bacteria causing the infection is used to identify which phage/s from available phage libraries can treat it. When matching phage/s are identified they are cleaned thoroughly so that they can be safely given to humans.
Different phages can be combined in a mixture called a phage “cocktail” which is then delivered in different ways depending on where the infection is, including by needle (intravenous), topically (applied to the skin) or by aerosol (nebulisation).
Phage therapy has been used in some cases overseas to successfully treat infections of the skin and lungs. In Australia, Phage Australia have commenced phage therapy for compassionate use, which is being carried out at several sites Australia-wide, including here in WA. You can find out more about phage therapy for compassionate use here.
Here in WA, we are working towards running a large phage therapy clinical trial for people with antimicrobial resistant lung infections. However, we would love to hear from you even if you don’t have a lung infection that is caused by AMR bacteria. If you would like more information on The Wal-yan Centre’s work on phage therapy please email PHAGE@telethonkids.org.au or click here to register your interest.
Does Phage WA collaborate with other research teams?
Our research team at the Wal-yan Centre work side by side with research teams around the world. Phage WA are part of the national network of Phage Australia, working together to ensure the best possible outcomes for those suffering with AMR infections.
Where can phages be found?
Phage WA researchers have isolated phages from environmental sources, such as wastewater and freshwater. However, phages are abundant and can often be found wherever the bacteria they infect may be.
What are the advantages of phages compared to antibiotics?
Many antibiotics affect several bacteria, not just the one causing the infection. While beneficial they can cause unwanted side effects including an upset stomach. Phage therapy can work as a personalised treatment by specifically targeting the causative species of the infection with high precision. Phages also act upon bacteria that antibiotics cannot because they are either in a protective shell called a biofilm or have developed resistance.
Furthermore, phages will not damage other organs, like the liver or kidneys, which some antibiotics use over a very long time are known to do.
Are phages safe?
Phages are viruses and natural predators of bacteria. Humans routinely come into contact with them without being harmed.
Why aren’t phages in use already?
Phage therapy was discovered before antibiotics, but it was quickly replaced in most countries because antibiotics were easy to make. Phage therapy has continued in Eastern European countries where antibiotics were not readily available, and most early phage therapy research has been performed in these countries.
Are there phages ready for every type of bacterial infection?
A considerable amount of time is required to build a phage repository and generate the data needed to ensure the safe and effective use in humans. However, we have phages ready to be used against some of the highest priority bacteria. In collaboration with other research institutes all over the world working in this space, we can access phages against other dangerous bacteria.
Can phage treatment be used on areas other than the lungs?
Yes. Phages are specific to a bacteria and are not restricted to treat infection in only specific areas/ organs of the body. Phages effective against AMR bacteria isolated from the lung have been shown to be just as effective in treating the same bacteria that causes skin infections.
Who will be eligible for phage therapy in WA?
To begin, phage therapy will be available to those recommended by a doctor. Specifically, individuals without viable treatment options, including those whose infections are not being cleared by currently available antibiotics, or those who are allergic to antibiotics.
Once phage therapy becomes more established, it can become more widely available by conducting clinical trials where interested participants can enrol.
Will people with normal lung function but suffer haemoptysis regularly, be able to be considered for phage therapy?
Phage therapy will be prioritised by people with the most serious lung infections. The selection criteria that clinicians consider include: lung function level, infection response to antibiotics and any antibiotic toxicity being experienced.
Eventually, phage therapy will be expanded to others who may be less clinically severe but still require other treatments.
What monitoring and precautions will be taken to care for the well-being of the patient as a whole? For example, the patient's normal microbiome may be disrupted.
Their immune system may need to be supported until the microbiome is restored. Extra precautions are taken to ensure phages are safe before they are even considered for therapy.
This includes looking at a phage’s genetic makeup, ability to kill bacteria and effects on human cells. Phages are specific for the bacteria they target, so they should not affect the rest of a person’s microbiome. They will also assist the immune system in removing a bacterial infection.
Phage therapy has been successfully performed in other countries without adverse events. Still, because it is not common practice, patient safety monitoring will be above what is currently achieved for antibiotics
How will phages affect current treatments?
Phage therapy will not replace antibiotics or any other treatments being provided. In fact, phages and antibiotics have been shown to work very well together and provide better treatment than either treatment alone.
Phages may also extend the usefulness of antibiotics by preventing resistance development over time.
Have there been any known side effects documented?
There have not been any serious side effects associated with phage therapy to date. The most serious side effect was when a patient experienced wheezing, shortness of breath, and fever controlled by medical staff.
What costs will there be for using this therapy?
Costs will vary depending on the type of infection that is being treated and how long the treatment will continue for. While the cost of phage therapy may seem high initially, when we consider the costs of trying to treat ongoing infections with treatments that are no longer effective, a single course of phage therapy is likely to be cheaper in the long run.
How long will it be before we can access phage therapies?
The first use of phage therapy in WA will be in those recommended by a doctor, either because they have infections that cannot be treated by antibiotics or because they have developed allergies that limit their treatment options.
Clinical trials will soon be underway to capture large-scale safety and effectiveness data which are necessary to make phage therapy more broadly used and available.