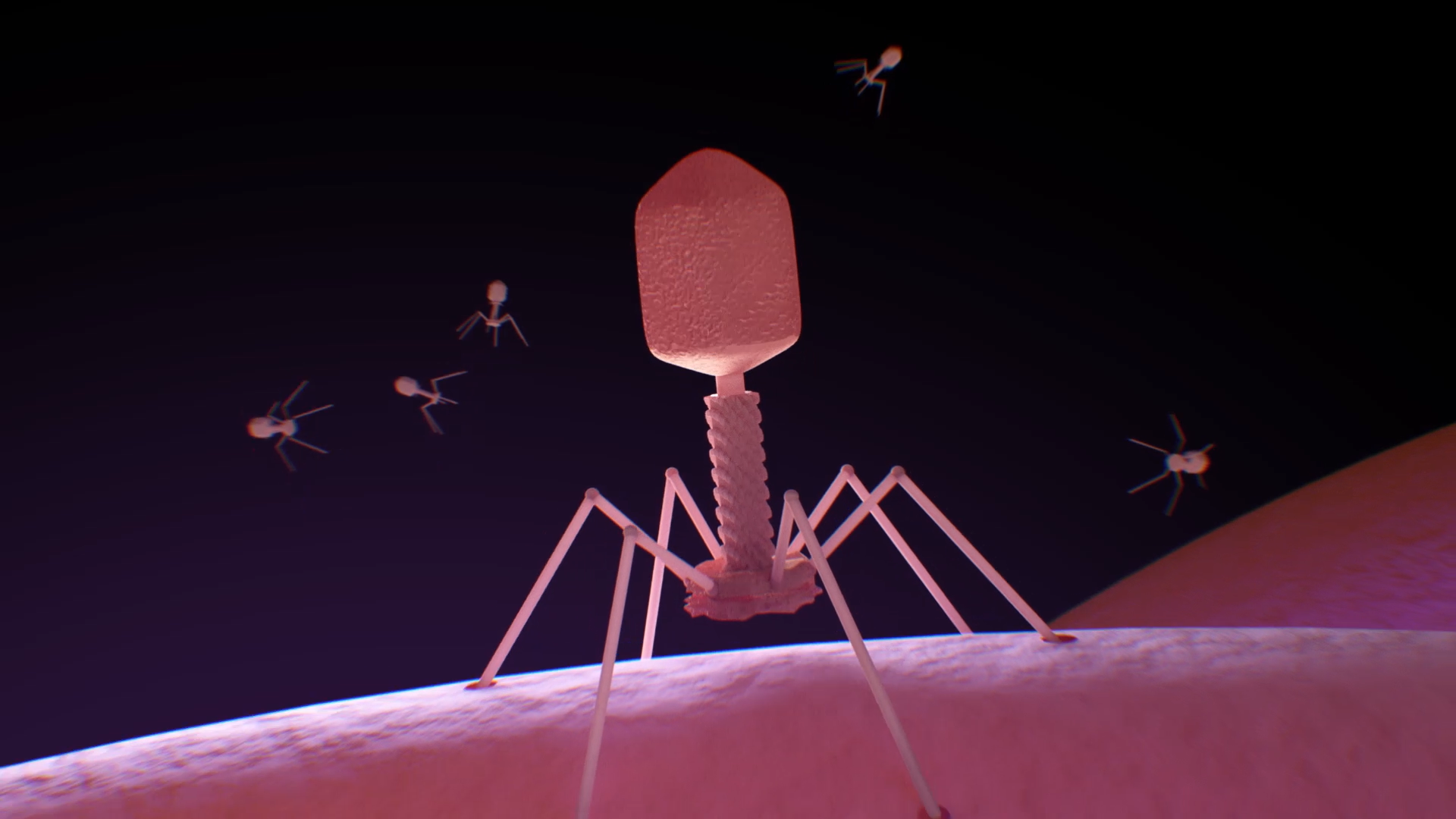
Phage WA have a number of projects underway and these cover a broad range of phage research areas.
At the Wal-yan Respiratory Research Centre we have a collection of >3,000 phages specific for Pseudomonas aeruginosa and Staphylococcus aureus and this collection has influenced much of our ongoing research. We are always expanding the range of target bacteria in our collection, based on advice from Infectious Diseases specialists at WA hospitals.
Publications of this work can be accessed at the below links, and some of our current projects have been showcased below.
Publications
‘Complete genome sequence of Burkholderia cenocepacia bacteriophage Karil-mokiny-1’
Jack S. Canning, Kak-Ming Ling, Daniel R. Laucirica, Joshua J. Iszatt, Stephen M. Stick, Anthony Kicic
A complete genome of an obligately lytic Pseudomonas aeruginosa bacteriophage, Minga-mokiny 4
Phoebe Carr, Kak-Ming Ling, Joshua Iszatt, Matthew Poh, Erika Sutanto, Renee Ng, Barbara Chang, Stephen Stick, Anthony Kicic
Jack Canning, Daniel Laucirica, Kak-Ming Ling, Mark P. Nicol, Stephen M Stick, Anthony Kicic
Joshua J Iszatt, Alexander N Larcombe, Luke W Garratt, Stephen M Stick, and Anthony Kicic
Stability Considerations for Bacteriophages in Liquid Formulations Designed for Nebulization
Rohan Flint, Daniel R Laucirica, Hak-Kim Chan, Barbara J Chang, Stephen M Stick, and Anthony Kicic
Pulmonary bacteriophage and cystic fibrosis airway mucus: friends or foes?
Kak-Ming Ling, Stephen Michael Stick, and Anthony Kicic
Genome Sequences of Two Lytic Staphylococcus aureus Bacteriophages Isolated from Wastewater
Joshua J Iszatt, Alexander N Larcombe, Luke W Garratt, Stephen M Stick , Patricia Agudelo-Romero, and Anthony Kicic, on behalf of WAERP and AREST CF
Genome Sequence of a Lytic Staphylococcus aureus Bacteriophage Isolated from Breast Milk
Joshua J Iszatt, Alexander N Larcombe, Luke W Garratt, Stephanie Trend, Stephen M Stick , Patricia Agudelo-Romero, and Anthony Kicic, on behalf of WAERP and AREST CF
Renee N Ng, Anna S Tai, Barbara J Chang, Stephen M Stick, Patricia Agudelo-Romero, and Anthony Kicic, on behalf of WAERP and AREST CF
Andrew Vaitekenas, Anna S Tai, Joshua P Ramsay, Stephen M Stick, Patricia Agudelo-Romero, and Anthony Kicic, on behalf of WAERP and AREST CF
Daniel R Laucirica, Stephen M Stick, Luke W Garratt, and Anthony Kicic
Ameneh Khatami, David A Foley, Morgyn S Warner, Elizabeth H Barnes, Anton Y Peleg, Jian Li, Stephen Stick, Nettie Burke, Ruby C Y Lin, Julia Warning, Thomas L Snelling, Steven Y C Tong, and Jonathan Iredell, on behalf of Phage Australia Clinical Network
Phage Therapy for Multi-Drug Resistant Respiratory Tract Infections
Joshua J. Iszatt , Alexander N. Larcombe, Hak-Kim Chan, Stephen M. Stick, Luke W. Garratt and Anthony Kicic
Pseudomonas aeruginosa Resistance to Bacteriophages and Its
Prevention by Strategic Therapeutic Cocktail Formulation
Andrew Vaitekenas, Anna S. Tai, Joshua P. Ramsay, Stephen M. Stick and Anthony Kicic, on behalf of AREST CF
Renee N. Ng, Anna S. Tai, Barbara J. Chang, Stephen M. Stick and Anthony Kicic
Renee N. Ng, Lucinda Grey, Andrew Vaitekenas, Samantha McLean, Jack Rudrum, Daniel Laucirica, Matthew Wee-Peng Poh, Jessica Hillas, Scott Winslow, Joshua Iszatt, Thomas Iosifidis, Anna Tai, Patricia Agudelo-Romero, Barbara Chang, Stephen Stick and Anthony Kicic, on behalf of AREST CF