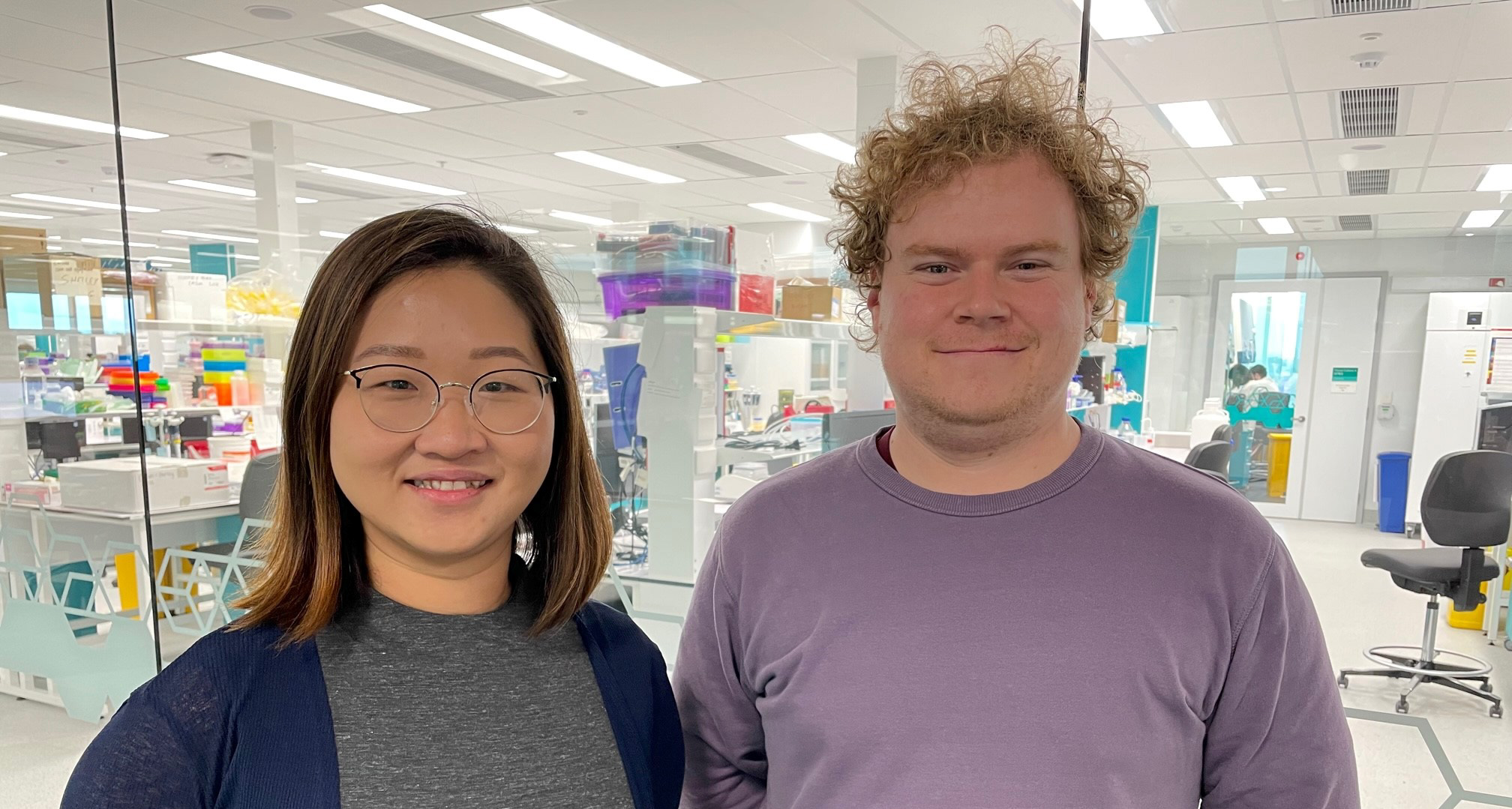
Two outstanding researchers from the Wal-yan Respiratory Research Centre, Dr Kak-Ming Ling and Dr Samuel Montgomery have been awarded Vertex Cystic Fibrosis (CF) Mentored Innovation Research Awards.
The Wal-yan Respiratory Research Centre is a powerhouse partnership between The Kids Research Institute Australia, Perth Children’s Hospital Foundation and Perth Children’s Hospital.
Together Dr Ling and Dr Montgomery have received funding to the value of $356,701(AUD) to support their innovative and collaborative clinical research to improve the care of people with CF.
The Vertex CF Research Innovation Awards are highly competitive grants created to inspire and support the next generation of M.D.s and Ph.Ds. who are working to advance the understanding of CF. The Mentored Research Innovation Awards provide grants of up to $125,000 USD distributed over two years to support mentored projects with established CF researchers.
Dr Ling, who will be mentored by Professor Stephen Stick and Associate Professor Anthony Kicic, received $178,798 (AUD) in support of her research entitled ‘Investigating Bacteriophage Behaviour and Efficacy in the Cystic Fibrosis Lung Microenvironment’.
Dr Ling said that young children with CF produce thick, sticky secretions (mucus) in their lungs, which prevent the lungs from working efficiently, thus making breathing difficult. Early antibiotic treatment to limit bacterial infections in the CF airways permanently alters the airway microenvironment, resulting in antimicrobial resistance (where bacteria have changed and cannot be killed by the antibiotics).
“Since there is little investment currently in discovering new antibiotics, alternative therapies need to be explored. Phage therapy is currently being investigated as one such alternative, and although various studies have assessed the relationship between phages and bacteria, the interaction between phages and host cells or their by-products, including mucus, is less known,” said Dr Ling.
Very recent evidence suggests that phages bind to aspects of mucus which improves their ability to kill bacteria. However, little is known about how the CF lung microenvironment impacts phage functionality, so this is what my research will investigate.
Outcomes from Dr Ling’s two-year research project will provide valuable information for future application of phage therapy for people with CF, regarding phage efficacy, administration route, and phage formulations.
Dr Montgomery, who will be mentored by Professor Stephen Stick, received $177,903 (AUD) in support of his research study which aims to improve the lung health of young children with CF following a viral infection.
Dr Montgomery said rhinovirus infection (the “cold” virus) is common in young children, often resulting in presentation to hospital emergency departments. This is worsened in children with CF where rhinovirus infection often results in deteriorating lung health, which is often permanent and leads to chronic bacterial infection and increased hospitalisation.
“Rhinovirus infects the cells lining the airway, provoking a large inflammatory response, which can lead to lung damage.
“Our team has previously identified a specific type of inflammation associated with decreasing lung health in children with CF. Through our research, we propose to block this inflammation using repurposed medication already approved for use in other diseases as anti-inflammatory treatments for the “cold” virus in children with CF,” said Dr Montgomery.
“Using a model of the airway in the laboratory, we will test the safety and effectiveness of these medications to reduce the inflammation following common viral infections.”
This study aims to provide evidence to progress to a clinical trial, as these medications are already approved for use in other diseases and could be rapidly translated into clinical use for children with CF. Congratulations to Dr Ling and Dr Montgomery for being awarded these highly competitive grants.